Abstract
Introduction
The direct antiglobin test (DAT) is a highly sensitive method (92 to 97%) for the diagnosis of autoimmune hemolytic anemia (AIHA). The diagnosis of DAT-negative AIHA (DN-AIHA) is one of exclusion but the definition of DN-AIHA is not consensual and guidelines on the minimal set of tests that should be performed to rule out other causes of hemolysis are lacking. In this study, we report the baseline characteristics and outcome of a series of both adult and pediatric cases of presumed DN-AIHA based on pre-defined diagnostic criteria. The main characteristics of adult' DN-AIHAs have also been compared with those of adult patients with a DAT positive warm AIHA (wAIHA).
Methods
Patients aged ≥ 5 years with presumed AIHA and negative DAT test performed with an anti- IgG, anti-C3, anti-IgM and an anti-IgA by column agglutination method were retrospectively recruited in France throughout the network of the French national referral center for adult' immune cytopenias and the screening of DAT results in 2 referral laboratories from the French Blood Centre.
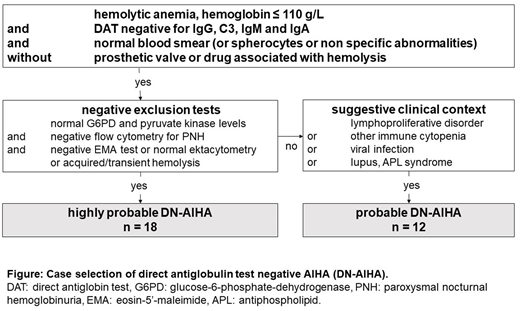
DN-AIHA cases were defined as highly probable (negative extensive work-up) or probable (negative minimal work-up but underlying compatible context, see Figure). Response to therapy was defined as complete (CR, hemoglobin (Hb) ≥ 120 g/L and no features of active hemolysis), or partial (PR, Hb ≥ 100 g/L, with an increase of at least 20 g/L from baseline and persistent hemolysis) in the absence of any recent transfusion. Adults with primary DN-AIHA (i.e, the cases) were compared to wAIHA controls recruited from the database of the national referral center (matched on age and gender) in a 1 to 2 ratio. Mann-Whitney and Fisher exact tests were used for the comparisons.
Results
In total, 23 adults (median age 61 years [range 19-86]) and 7 children (15 years [7-17]) with a male/female ratio of 1.5, diagnosed between 2003 and 2018, were included. All of them fulfilled the pre-defined inclusion criteria (18 highly probable, 12 probable DN-AIHA).Most DN-AIHA (57%) were secondary and associated to an underlying disease including: a clonal lymphoproliferative disorder (n=9), a myelomonocytic leukemia (n=2), a viral infection (n=3), an ulcerative colitis (n=1), a primary immune deficiency (n=1), an antiphospholipid syndrome (n=1). DN-AIHA was associated with another immune cytopenia in 4 patients (immune thrombocytopenia in 3).At diagnosis, the median hemoglobin level was 71 g/L [28-96], the reticulocyte count 221 G/L [79-500], the total bilirubin 51 µmol/L [8-221], the LDH 1.6 times the normal level [1-6]. Hemoglobinuria was reported in 8 patients. Spherocytes and red blood cell aggregates were observed on the blood film in respectively 9 and 2 patients. Most patients (83%) required red blood cell (RBC) transfusion and received a total of 8 [1-70] RBC packed units, and up to 5 [1-39] per month.
Twenty eight patients (93%) received corticosteroids. The overall initial response rate was 82% (CR in 25%, PR in 57%) but a relapse occurred at tapering in 65% (at a median daily dose of 15 [10-40] mg of prednisone). A second-line treatment was required in 62% including: rituximab (n=17, R in 33%), immunosuppressors (n=4), splenectomy (n=3, CR in 2), treatment of associated clonal disorder (n=3; polychemotherapy, azacitidine, ibrutinib; R in 100%). After a median follow-up of 54 weeks, 10% of patients had died due to progression of malignancy (n=2) or infection (n=1), whereas 30% were in complete remission.
The baseline biological parameters, the overall response to corticosteroids did not differ significantly between adult with primary DN (n=10) and wAIHA (n=20). However, patients suffering from DN-AIHA required more RBC packed units than DAT-positive wAIHA (p<0.05).
Discussion
DN-AIHA is a rare condition that remains a diagnostic challenge since it requires an extensive negative work-up to rule out any other cause of congenital or acquired hemolytic anemia. Next Generation Sequencing analyses are now increasingly used to detect the presence of relevant variants and somatic mutations and may be helpful to sort out some previously unexplained hemolytic anemia. Consensual definition criteria for DN-AIHA are needed to avoid misdiagnosis and the use of inappropriate therapies. The management of DN-AIHA is not standardized and mostly extrapolated from the one of wAIHA. Steroids, splenectomy and/or the treatment of an underlying disease may lead to a complete and durable remission.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal